Americans are divided over the distribution and severity of the Covid-19 virus. A wide swath of Americans view the virus as a variant of flu with its dire effects greatly overstated. On the other hand, mainstream public health officials and establishment media emphasize the dangers and risks of the virus and its threat to health and well-being. What is the reality?
The US Experience
A problem in sorting out the reality is sudden and devastating waves of infection that afflicted Italy, Spain, France, the UK, and the Northeastern US. Covid-19 was easily transmissible and quickly afflicted large numbers of people. Hospitals were overwhelmed. Elderly individuals were the bulk of patients, but also affected were younger and middle-aged persons with pre-existing health issues.
Americans were facing this crisis with little sense of what awaited and little control over the outcome. In an environment of unknowing, theories abound. Early estimates of the lethality of Covid-19 Case Fatality Rate (CFR) based on hospital records and afflicted cohorts varied from 2 percent to 6 percent. For many especially the elderly and persons with preexisting health conditions, Covid-19 seemed like a death sentence.
In the US, testing and contact tracing to limit the spread of the disease that had been implemented with great success in China, Hong Kong, Singapore, New Zealand, Australia, Finland, and other European countries lagged. The Centers for Disease Control and Prevention (CDC) seemed ill-prepared. The administration largely ignored the early stages of the infection as it took root in the US.
Viral Reproduction (R0 ), Case Fatality Rate (CFR), Infection Fatality Rate (IFR)
To appreciate the arguments put forward by different sides in this debate, some definitions are important. R0 or R zero is the basic reproduction rate that conveys the expected number of cases generated by one person among susceptible individuals. R0 less than 1 means a diminishing number of persons infected, and R0 greater than 1 means an increasing number. Case Fatality Rate (CFR) is the proportion of deaths from a disease in relation to the total number of people diagnosed with the disease. The Infection Fatality Rate (IFR) represents the proportion of deaths in relation to the total number of people infected by the disease. The CFR is based upon diagnosed cases solely while the IFR includes diagnosed, undiagnosed, and asymptomatic infections.
Infection Fatality Rate
Early in the pandemic, estimates of death following infection varied between 2.4 to 5.4 per hundred, mirroring the Case Fatality Rate (CFR). Gradually, studies began to appear in districts and cantons of Italy and Switzerland that suggested up to 10 times the number of persons than had been hospitalized had serological evidence of previous infection and experienced no symptoms. In the same vein, about half the infected passengers quarantined on the Princess Cruise Ship were symptom free. As more people were identified with the virus, epidemiologists began to ratchet down the Infection Fatality Rate (IFR) of Covid-19. Following inclusion of undetected cases, the IFR is now generally agreed to range from 0.06 to 0.10 per hundred across age groups. The revised estimates are still grim and compare with the average seasonal flu IFR that hovers around .01. The Infection Fatality Rate (IFR) suggests that Covid-19 is 6 to 10 times more deadly than the flu.
US 2020 Influenza Deaths
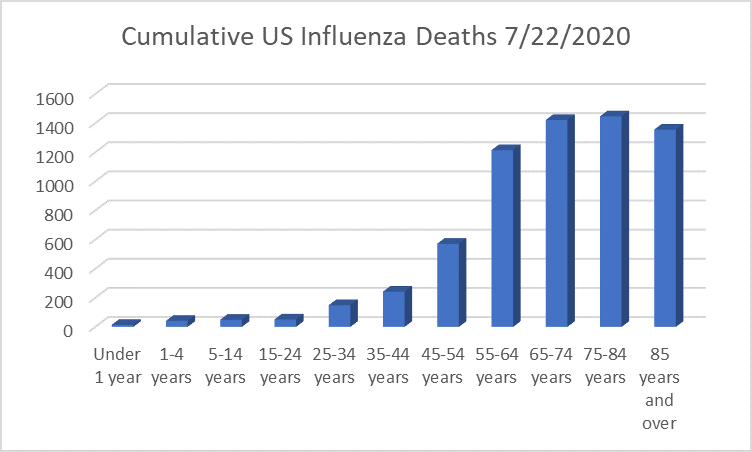
Figure 1: Cumulative US Influenza Deaths by Age Group. Data compiled from the CDC database.
The total number of influenza cases from January 1st to July 22, 2020 is 6,553. The median value for influenza deaths per year during the past five years is 38,230. The current value is well below expectations, perhaps due in part, to following public health guidelines that limit aerosol and droplet transmission, and to vulnerable individuals succumbing to the more infectious Covid-19. Influenza’s Reproduction Rate (R0) is calculated between 0.9 and 2.1 in contrast to Covid-19’s with values between 2.2 and 2.7. Like Covid-19, however, influenza more grievously afflicts persons with pre-existing conditions, the middle aged, and the elderly.
US 2020 Covid-19 Deaths
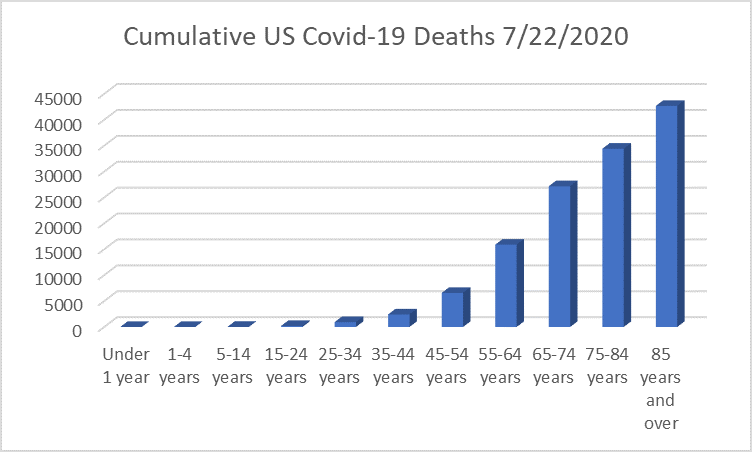
Figure 2: Cumulative US Covid-19 Deaths by Age Group. Data compiled from the CDC database.
The total number of US deaths attributed to Covid-19 through July 22, 2020 was 143, 868. The CDC updated the number one week later on July 28, 2020 to 147,672. Covid-19 deaths gradually ramp up beginning in the 20-year-old group then rise exponentially starting in the 45 to 54-year-old group. The rise continues into old age even as populations in later cohorts’ decline.
The reasons for the observed Covid-19 distribution of deaths by age profile are various. As persons age, immune response declines. The number and severity of chronic disease increase. Older persons are increasingly likely to be in retirement homes or managed care facilities which have become Covid-19 “hotspots”, and potent vectors for disease transmission.
Preexisting Health Conditions and Covid-19 Deaths
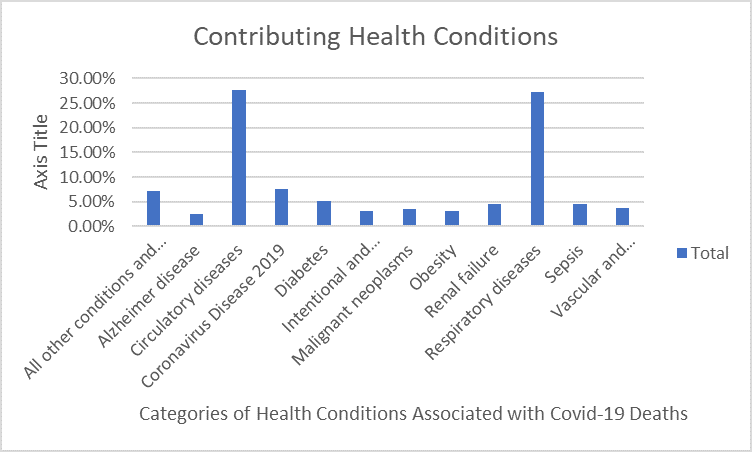
Figure 3: Percent Distribution of Health Conditions Associated with Covid-19 Deaths Note: The data is based upon 8,060 death certificates filed by US states with the CDC. The distribution of major categories of pre-existing conditions associated with Covid-19 deaths is complete through July 22, 2020. The report reflects a fraction of deaths due to differences in filing time and compliance. The CDC offers more refined data about causes of death, including ICD diagnoses, through a spreadsheet available at its website.
In order of severity, the major categories of preexisting health conditions related to Covid-19 deaths identified by the Centers for Disease Control and Prevention are Alzheimer’s Disease (2.55%), obesity (3.11%), intentional and unintentional injury (3.09%), malignant neoplasms (3.57%), vascular and unspecified dementia (3.7%), renal failure (4.48%), sepsis (4.55%), diabetes (5.13%), other causes (7.2%), corona virus disease (7.66%), respiratory diseases (27.3%), and circulatory diseases (27.67%). Clearly, circulatory, and respiratory disorders are in the foreground followed by diabetes and associated complications. The presence of Alzheimer’s and dementias reflect the high incidence of deaths among older persons in assisted living facilities. But any condition that compromises immune function increases the likelihood of death.
Racial and Ethnic Covid-19 Disparities
Black and Hispanic Americans are more likely to be infected by Covid-19, hospitalized, and die than white Americans. Depending upon locality, Black and Hispanic Americans are twice to three times more at risk. Members of these groups are more exposed to infection by virtue of living arrangements, occupation, and forms of social interaction. Exposure is often compounded by pre-existing health conditions, such as diabetes, obesity, and emphysema. Health care for chronic conditions may be marginal or unavailable due to absence of local facilities, poverty, or immigration status.
Estimated Number of Asymptomatic (Subclinical) Covid-19 Infections
Since the Infection Fatality Rate (IFR) from Covid-19 now includes asymptomatic individuals, and spans the young and the old, the number of persons who have been infected may be calculated from the number of deaths. The CDC lists the current total number of deaths from the virus in the US on July 22, 2020 as 143, 868 persons. If the IFR equals 0.06, only 6 percent of all infected persons are represented. Adding the additional 94 percent yields a total of 13,667,460 persons or 4.1 percent of the US population. If the IFR equals 0.10, adding the additional 90 percent yields a total of 13,091, 978 persons or 3.9 percent of the US population. This contrasts with the CDC infection count of 4,024,492 or 1.2 percent of the US population. The estimate of infected persons is roughly 3.25 times larger than the confirmed infection count.
At the time of this writing, excess deaths from all-cause mortality during the period of the Covid-19 pandemic is 28 percent higher than that attributed to Covid-19 on death certificates. If this 28 percent increment is added to the official count of Covid-19 deaths when the IFR equals 0.6%, the total number of infected persons rises to 17,309,934 persons or 5.1 percent of the US population, and when the IFR is 1% , the total number rises to 16,757,468 or 5.0 percent of the US population.
Evidence for Both Sides of the Debate
Therefore, evidence supports both sides of the Covid-19 debate: Is Covid-19 as dangerous as authorities make it to be? On the one hand, many more persons are infected and likely asymptomatic than persons with symptoms, and those who are under 35 years of age, unless compromised by preexisting conditions, run a marginal risk of illness. On the other hand, Covid-19 is highly infectious, including those who are asymptomatic, 6 to 10 times more lethal than the flu, increasingly dangerous with age, and often deadly when coupled with preexisting conditions.
The back estimation of Covid-19 infections in the US makes clear that the virus has a long way to run with a potential fatality limit from 1,986.000 for 0.06 per hundred death rate to 3,310, 000 persons for a 0.10 per hundred death rate. Neither fatality limit is likely to be realized. Americans are widely dispersed. Increasing numbers practice social distancing, appropriate hygiene, avoid crowds and public transportation. Improved medical treatments and a potential vaccination are likely to further reduce the Infection Fatality Rate (IFR).
Long-Term Consequence of Covid-19 Infection
The lingering effects of Covid19 are largely unknown. Research with Sars1, a relative to Covid-19, aka Sars2, presents a bleak picture. Pulmonary problems, shortness of breath, and chronic fatigue characterized the aftermath of Sars1 infections for survivors. Survivors were relatively young at the time of infection, typically in their 20s or early 30s. Persons older at the time of Sars1 infection were less likely to survive at all.
Anecdotal evidence about the lingering effects of Covid-19 Is comprised of narratives from Covid-19 survivors about the aftermath of the virus. Like Sars1, shortness of breath, pulmonary issues, memory issues, and chronic fatigue are common themes. Clinical observation suggests the severity of aftermath is associated with the symptom pattern and duration of the infection. The COVID Symptom Study revealed six separate clusters of COVID-19 symptoms:
- (‘flu-like’ with no fever): Headache, loss of smell, muscle pains, cough, sore throat, chest pain, no fever.
- (‘flu-like’ with fever): Headache, loss of smell, cough, sore throat, hoarseness, fever, loss of appetite.
- (gastrointestinal): Headache, loss of smell, loss of appetite, diarrhea, sore throat, chest pain, no cough.
- (severe level one, fatigue): Headache, loss of smell, cough, fever, hoarseness, chest pain, fatigue.
- (severe level two, confusion): Headache, loss of smell, loss of appetite, cough, fever, hoarseness, sore throat, chest pain, fatigue, confusion, muscle pain.
- (severe level three, abdominal and respiratory): Headache, loss of smell, loss of appetite, cough, fever, hoarseness, sore throat, chest pain, fatigue, confusion, muscle pain, shortness of breath, diarrhea, abdominal pain.
Current research and clinical observation support the association between severity, from 1 to 6, and lingering effects. Some effects appear not readily reversible. However, a cautionary study by German investigators titled “Outcomes of Cardiovascular Magnetic Resonance Imaging in Patients Recently Recovered From Coronavirus Disease 2019 (COVID-19)” published the July issue of Jama Cardiology calls into question the clinical observation of association between severity and long-term effects. Magnetic resonance imaging (MRI) scans of 100 persons who recovered from Covid-19 at home or at a hospital showed 78% with cardiac involvement and 60% with myocardial inflammation. No relation existed between symptom severity and preexisting conditions and the overall course of the acute illness or the time from the original diagnosis. These cautionary findings have relevance as well to persons who were positive for Covid-19 and asymptomatic
Lingering Effects of Asymptomatic Infection
Forty to eighty percent of the population infected by Covid-19 may be asymptomatic. If the median back estimate of 4.5 percent of the US population is correct, and half are asymptomatic, the number is 7,447,500 asymptomatic persons. Many of this group are likely under 35 years of age and free from conditions that contribute to the severity of the disease. For this age group, long-term effects are likely to be muted. But as age and contributing conditions ratchet up, the likelihood of damage, even for infected persons without symptoms, increases. The 20 to 60 percent of persons who display symptoms and as many as half without symptoms are likely to experience a decreased quality of life. This is due to stealth damage to the lungs, circulatory system, kidneys, brain, and other organs.
The literature concerning asymptomatic Covid-19 infection is limited. In a paper published in March, 2020 in the journal Radiology titled “Chest CT Findings in Cases from the Cruise Ship “Diamond Princess” with Coronavirus Disease 2019 (COVID-19)”, Shohei Inui et al evaluated computed tomography (CT) scans of lung and bronchial passages of 104 persons who were quarantined on the Diamond Princess Cruise Ship. A total of 104 cases were examined, 76 of whom were asymptomatic and 28 symptomatic. The authors concluded,
“Although lung parenchymal and airway abnormalities were more frequent in symptomatically than asymptomatic cases, noticeably, we found lung parenchymal changes on CT in up to 54% of the asymptomatic cases. In those who showed CT abnormalities, asymptomatic cases showed significantly (sic) predominance of GGO, while consolidation was predominant in symptomatic cases.”
Glass Opacity (GGO) describes the tissue damage in the lungs of asymptomatic volunteers. GGO is used in chest radiography to refer to a region of hazy lung radiopacity, often diffuse, in which the edges of the pulmonary vessels may be difficult to distinguish. GGO is indicative of infection, chronic interstitial disease, acute alveolar disease, and other chronic and acute syndromes.
At the same time, the results of the paper support the view that lung damage is linked to the severity of symptoms during infection with half (54%) of asymptomatic patients having lung damage. The more severe the symptoms, the more severe the aftermath, but absence of symptoms did not mean absence of aftermath. The disease may be subclinical, but consequences are observed that likely impact the future quality of life.
Confused Public Policy
Among developed nations, the US has fallen far behind in control of the virus. US prestige and soft power has been eroded. A country that cannot manage itself cannot claim to manage or lecture other countries on how to manage themselves.
A window into “behind the scenes” influence that may have contributed to the US stumbling response to the Covid-19 virus were early prognostications by a group of epidemiologists, savey academics, and thought leaders. John Ioannidis, a Stanford professor, appeared to play a pivotal role in demoting the threat level of Covid-19 to little more than the seasonal flu. An early study (March, 2020) of Covid-19 seroprevalence led by his team concluded the Infection Fatality Rate (IFR) at 0.012 to 0.02 and later revised to 0.017. The study, a focus of Op Ed columns in the Wall Street Journal and the New York Times provoked controversy among specialists due to its design and possibility of false positives that would reduce estimated IFR. More recently, Ioannidis has provided an update to his earlier estimation based upon a review of published seroprevalence data. He concluded that the overall Covid-19 IFR is 0.027, a relatively small shift from his initial estimate. However, the estimated IFR varies depending upon the ratio of deaths to population, Ioannidis writes,
“Median corrected IFR was 0.10% in locations with COVID-19 population mortality rate less than the global average (<73 deaths per million as of July 12, 2020), 0.27% in locations with 73-500 COVID-19 deaths per million, and 0.90% in locations exceeding 500 COVID-19 deaths per million.”
In other words, the higher the death rate, the higher the IFR. By the end of August, US deaths from Covid-19 deaths are likely to equal or exceed 500 per million. Many metropolitan areas already meet this criterion. The US IFR at 0.90% is 4 1/2 to 7 1/2 times Ioannidis et al’s earlier estimation of 0.12% to 0.2%
Where to from Here?
As the quality of life decreases, so does economic productivity. Dependency and the demand for services increase. The cost of Covid-19 has yet to be calculated and perhaps will never be known. Presently, the US preoccupation is the current costs of support for individuals, families, and businesses deprived of income. But cost is long-term. In an economy that expects 2-3% growth as a norm, the weight of Covid-19 costs is likely to continue and weigh upon productivity from Covid-19’s sequelae.
Lessons learned from the Covid-19 debacle are sobering and suggest different priorities in the national debate about the future course of government policy. The first lesson is lack of foresight and preparation is costly. Money does not substitute for intelligence. Contingency planning is essential. Government must reexamine its priorities. The physical health of its citizenry undergirds social and economic well-being. Public Health needs to be revamped. The second lesson is the economic interdependence of Americans. The country cannot be shut down without profound effects on individuals, families, and businesses.
Pseudoscience and conspiracy theories that characterize Covid-19 risks as “fake” are a strategy to minimize public concern and resume everyday activities. Early in the pandemic, the Infection Fatality Rate (IFR), based on selected observations, was set unrealistically low. Whether to follow public health recommendations was cast as an intrusion into individual rights. Many young adults embraced these arguments, and, in fact, death rates for young adults are only 2 to 2 1/2 times the number of those who die from influenza during a typical season. The majority in the age group are asymptomatic although the illness is unpleasant, so relatively few young adults had acquaintance with the disease –although with rising infections in Florida, Texas, Arizona, and Southern California, this may be changing.
An economic strategy that throws older citizens and minorities under the bus by prematurely opening the country, after bungling Covid-19 containment, undermines the covenant of democracy to seek the common good. The strategy is callous, to say the least, and appeals to narrow self-interest, so long as it is one’s neighbor and not oneself who is infected.
This time of Covid-19 infection is not only a time to review and revamp public health, but a time to reflect and review our relation to our neighbors and what it means to be a member of a community of people that share a common humanity.
